Navigating the intricate world of healthcare administration can often feel like a complex puzzle, especially when it comes to ensuring that all medical professionals are properly vetted and authorized to provide patient care. This essential process, known as provider credentialing, is the bedrock of patient safety and organizational integrity. Without a robust system in place, healthcare entities risk non-compliance, financial penalties, and, most importantly, compromising the trust placed in them by patients.
To streamline this critical function and bring much-needed clarity to the often-daunting task, many organizations are looking for a comprehensive guide. This is where a well-structured provider credentialing scope of work template becomes an invaluable asset. It acts as a detailed blueprint, outlining every step, responsibility, and expectation involved in the credentialing lifecycle, from initial application to ongoing monitoring.
By clearly defining the scope, healthcare facilities, credentialing specialists, and even individual providers can understand their roles, deadlines, and the precise requirements needed for successful credentialing. This not only enhances efficiency but also ensures consistency, reduces errors, and ultimately supports a safer, more reliable healthcare environment for everyone involved.
Why a Defined Scope of Work is Crucial for Credentialing Success
Having a meticulously crafted scope of work for your credentialing processes isn’t just a matter of good organization; it is absolutely fundamental to the operational health and legal compliance of any healthcare entity. It brings a level of clarity and structure that can transform what might otherwise be a chaotic and error-prone undertaking into a smooth, predictable, and highly efficient operation. This document serves as an anchor, guiding every action and decision within the credentialing department.
Firstly, a well-defined scope ensures unwavering compliance with regulatory bodies and accreditation standards. Healthcare is a highly regulated field, with organizations like NCQA, URAC, and state licensing boards setting stringent rules for provider qualifications. A clear scope of work translates these complex regulations into actionable steps, minimizing the risk of oversight and the severe penalties that can accompany non-compliance, protecting both the organization and its patients.
Secondly, it dramatically improves efficiency and reduces administrative burden. When every team member knows their specific responsibilities, the required documentation, and the sequence of tasks, bottlenecks are minimized. This prevents redundant efforts, ensures that all necessary information is collected in a timely manner, and allows for a more rapid turnaround time for credentialing applications, getting providers ready to serve patients faster.
Thirdly, it fosters accountability and provides a framework for performance measurement. With a clear scope, individual and team performance can be accurately assessed against defined metrics. This transparency empowers management to identify areas for improvement, implement targeted training, and optimize resource allocation, leading to continuous enhancement of the credentialing process. It also acts as an invaluable training tool for new staff, quickly bringing them up to speed on the intricacies of the department.
Key Components to Include in Your Scope of Work
To create an effective and all-encompassing provider credentialing scope of work template, it is vital to detail specific elements that cover the entire lifecycle of a provider’s association with your organization. Neglecting any of these crucial areas can lead to gaps in your process and potential compliance issues.
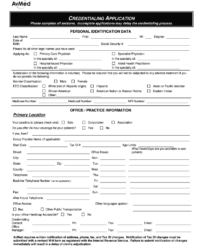
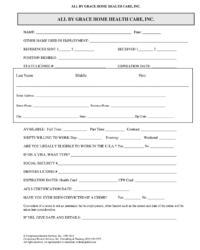
- Applicant Information Collection: This segment outlines how initial applications are gathered, what forms are used, and the preliminary data verification steps. It also covers secure storage and handling of sensitive personal and professional information.
- Primary Source Verification (PSV): Detail the exact procedures for verifying credentials directly from their original sources, such as medical schools, licensing boards, certification agencies, and past employers. Specify turnaround times and documentation requirements for each verification type.
- Committee Review Process: Describe the composition of the credentialing committee, their roles, responsibilities, and the established protocols for reviewing applications, making recommendations, and approving or denying privileges.
- Maintenance and Recredentialing Schedules: Outline the ongoing monitoring processes, including license expiration tracking, continuous query of sanction databases, and the systematic schedule for recredentialing providers at regular intervals, typically every two or three years.
- Reporting and Documentation Standards: Specify how credentialing data is documented, stored, and reported. This includes outlining audit trails, maintaining digital and physical records, and generating reports for internal review or external regulatory bodies.
- Roles and Responsibilities: Clearly delineate who is responsible for each step in the credentialing process, from administrative support staff to credentialing specialists, medical staff leadership, and the governing board. This eliminates ambiguity and ensures ownership.
Implementing and Customizing Your Credentialing Template
While a generic provider credentialing scope of work template can offer a solid starting point, true success lies in its careful implementation and thoughtful customization to fit the unique ecosystem of your healthcare organization. No two facilities are exactly alike, and factors such as organizational size, specialty focus, geographic location, and specific regulatory environment will significantly influence the fine details of your credentialing needs. Therefore, think of the template as a robust framework that requires tailoring to truly unlock its full potential.
The customization process involves a thorough internal assessment of your existing workflows, identifying pain points, and understanding the specific requirements of your medical staff and the services you provide. Engage key stakeholders, including medical staff leadership, legal counsel, and the credentialing team itself, to gather insights and ensure that the tailored scope accurately reflects operational realities and strategic goals. This collaborative approach not only produces a more effective document but also fosters buy-in from those who will be using it daily.
Furthermore, integrating your customized scope of work with your existing technology solutions, such as credentialing software or electronic health record systems, is paramount for seamless operation. Automation, where appropriate, can significantly reduce manual tasks, minimize human error, and free up your team to focus on more complex aspects of verification and review. Regular training sessions for staff on the updated scope and technology integration will ensure consistent application and maximize efficiency across the board.
Creating and implementing a well-defined scope of work for provider credentialing is a strategic move that pays dividends in both operational efficiency and unwavering compliance. It transforms a complex administrative function into a clear, manageable process, safeguarding patient care and strengthening the foundation of your healthcare organization.
By embracing a comprehensive and customized approach to your credentialing processes, you empower your team with the tools needed to perform at their best, ensuring that every provider meets the highest standards of qualification. This commitment to excellence ultimately reinforces your organization’s reputation and its dedication to delivering safe, high-quality healthcare services.